Smart Service Power: A Case Study on Building a Successful IoT Aged Care Service
IoT offers great potential to transform society for the better, but where do you start? Bettina Horster from VIVAI Software illustrates the steps taken to develop a new IoT-supported solution for aged care.

© onlyyouqj | istockphoto.com
Smart Service Power is an IoT-enabled assisted living project designed to face the challenges of a growing aging population, and to enable elderly people to remain in their independent home environment for longer. This article outlines the process of developing the concept and the business model, of testing and selecting technological components, and of finding partners to create a vibrant IoT ecosystem.
Related Stories

Undertaken in partnership with a range of stakeholders in aged care – such as city administration, nursing service providers, and medical insurers – alongside software and smart home developers, research institutes, and associations, the Smart Service Power project seeks to leverage the Internet of Things in a way that protects patient autonomy and privacy, while also ensuring safety and well-being in a cost-efficient environment. The eco Association is a member of the consortium of stakeholders, with a particular interest in ensuring data protection and privacy within the service.
What makes the project special is its customer-centricity. The focus is placed on the customers’ needs, and not simply on what is technically feasible. When the project was initiated, the first step was to undertake a major piece of research into what is really important for aging people living alone, and what the needs of their relatives are.
Defining the Service – Three Categories of Use Cases for Assisted Living
The research revealed three categories of use cases that are extremely important for aging people who live independently. These are firstly, safety and secondly, intake, which relate specifically to the state and behavior of the person in question. The third category is cognition, which also has to do with how the system interacts with the person.
Safety
Looking first at safety, we can distinguish between both direct and indirect issues. It is necessary to detect a fall – as this is the situation that summons up the greatest fear for people. For this kind of monitoring, there needs to be dedicated fall sensors for the direct detection but also, for the purposes of indirect detection, there must be sensors in the rooms that can detect certain kinds of motion or lack thereof. For a close monitoring, both types of sensors are necessary. But it is also important, if not as immediately critical, to detect changes to vital data, and here, it may be necessary to affix a sensor directly to the person’s body – as in the example below.
Intake
The next category is about intake – fluids, food and medication – and here, what is especially important is that the person is hydrated. Elderly people lose the capacity to identify whether or not they are thirsty – and a major cause of hospitalization of older people is dehydration. As a result, it is very important to assess whether they have a sufficient intake of fluids. To achieve this in the Smart Service Power project, we make use of a little plaster that measures the tension of the skin. If the tension is too weak, this lets the system know that the person needs to drink water.
Following on from this is how aged patients take their medication. In our assisted living system, we have included a dispenser for medicine, and it has a face recognition technology so it can see who the person is and pinpoint what medication is needed for that particular person.
Cognition
The final category, cognition, encompasses the need to communicate via natural language with the system. This allows the system to give reminders and offer advice. This is critical because, even if people are totally stressed out, they know how to react when somebody approaches them with a question, or if someone says, “Are you ok?” in case of a fall detection, or “You have to drink some water”.
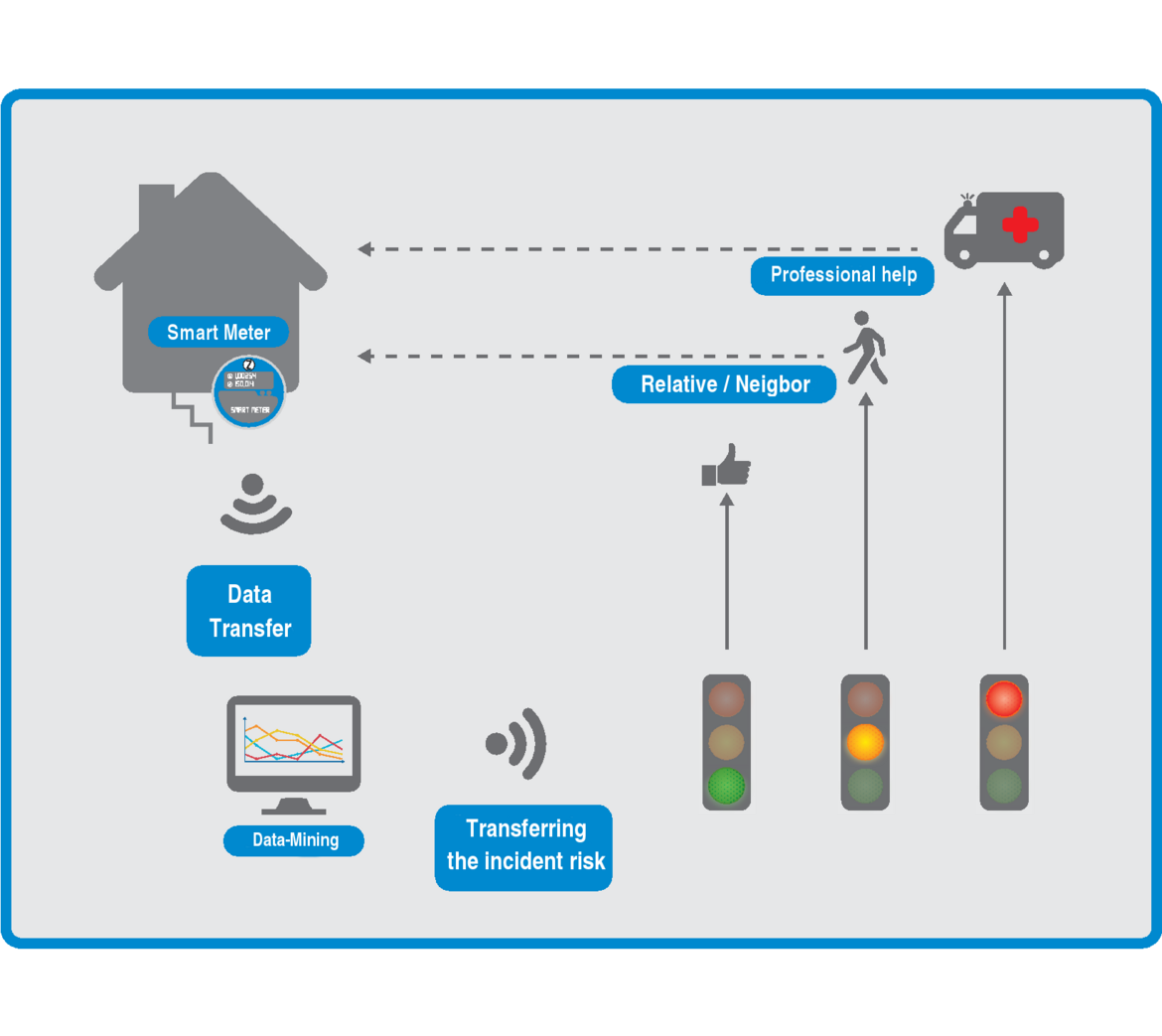
Looking outside of the immediate home environment, it is also necessary that designated relatives receive information on the condition of their parents or relatives. We have implemented a traffic light system with red, green, and yellow signals, and it provides information on whether the person in question is in good shape or whether something serious has happened, and whether the relative needs to call or take action.
These are examples of the basic information that we are gathering.
Integrating data sources – getting a holistic view
The data are all collected in one data platform and can be analyzed in relation to one another. For example, if a person gets a new medication and subsequently that person stays in bed far longer than normal, this change is registered. The nursing service can be alerted, the doctor spoken to, and the medication changed if necessary. There’s a machine-learning mechanism behind the system, and it learns the normal behavior and routines of this person. This means we don't simply get data, but we build profiles, and the profiles learn and improve over time.
Is it normal that this person was up all night and is this to be expected because they do it all the time? Or is this a person who used to sleep really well at night and has started to become restless, get up, and move around at night? That could be a sign for Parkinson's or for dementia, for example. The data can provide a warning signal that it is time to talk to the doctor.
Balancing Reliable Monitoring and Personal Privacy
All the sensors (aside from the plaster on the skin) are located in the house and not on the body. With other similar systems, it is normal for patients to need to wear a watch or a necklace, and to push a button to interact with the system. We think that it is not constructive to require people to do such things when they are stressed-out or in a panic, for example.
But, at the same time, it is important not to have a “big brother” approach. There are no cameras that submit pictures. You need to have these sensors in the bathroom, but nobody wants their privacy disturbed to such an extent. This means there is a need to use other sensors. One possibility we are researching is a technology called Time-of-Flight (ToF). Another really interesting type of sensor which we are looking into right now is a low-frequency radar system. This system is useful for detecting if somebody has fallen.
What is also different to other systems is the data usage control. This means that the user can elect who is going to be addressed if there's an emergency. And the user can decide that the data is only to be transmitted outside of the home in the case of an emergency. From the perspective of the potential of the service, this may not be ideal, because you don’t get machine learning and all the extra benefits of aggregated data – but there are people who just don't want it. The user can choose who has access to what data, and what they want to keep private, and this can be done at a very granular level. We want to give people the assurance that we don't mess with their data. And this, for me, is one of the most important features of the system, and that's what really stands out in comparison to other systems.
Choosing a platform
In the early stages of the Smart Service Power project, all the platforms available were quite new and we weren't really sure which one to take. As a result, we built up a set of 27 indicators (read dotmagazine interview "How to Choose the Right IoT Platform for Your Needs") to examine what's important about an IoT system. This research process was enormously helpful for our decision because, for example, we knew that we needed a natural language system, machine learning, and user modelling, and we wanted an open system.
Assisted living business models – Finding partners
At the outset of the project, we looked into all the ambient assisted living systems of the past 20 years, and they all failed – and we wanted to know why. It turned out the answer is really very simple. They didn't have a business model that really helped them to survive, because they were much too technically focused, and they didn't really have anybody but the aged residents who would pay for the service.
So right from the beginning, we worked together with the city of Dortmund and the city of Arnsberg, in the state of North Rhine-Westphalia, in order to ensure that they would participate in the business model. Because they are the ones who really have the most to gain in this whole area: If people stay in their homes longer, it is much less expensive for the cities than if they have to support people in homes for aged care. In Germany, communes have a legal requirement to support their citizens. And so, we wanted them to be in the consortium because we felt that they are really the big winners of the system.
Together with the city of Dortmund and the InHaus GmbH we asked ourselves how we can build a system which can really help to manage the demographic change. We looked at the value chain and wanted to have somebody on each step of the value chain. People were very enthusiastic about the system, so it was not that difficult. We found somebody at every stage of the aged care value chain.
The cities themselves think that a project of this nature is beneficial for them. Now, we are undertaking the design together with cities in Germany. We are designing our business model to be fair, meaning that everybody has to pay their fair share. Funding cannot simply be left to the people who use the service.
At first, only the city of Dortmund thought this way, but the more we talked about it and the more we worked together with politicians, the more they felt that it would be a good thing if a broad majority of people were able to participate in such a system. This way, it's not only for a privileged few who can afford the soft and hardware, the installation, and so on. As a result, we do a lot of lobbying in the project.
The stakeholders
So, in terms of stakeholders, you firstly have the communes, because they have to pay a lot of money into the social welfare system. There are a lot of people getting much, much older these days. With the demographic change in Germany, the cities are needing to prepare for a flood of people over 90 in the next 20 years.
And then there are also a lot of other stakeholders. First of all, the nursing services, which are really interested because it can be a revenue driver creating extra services. In a lot of cases it is the nursing service that is the first to get the emergency alarm, and who are approached if there is something wrong with the vital data, etc. Then you have the emergency services, which are clearly an important component of an aged care ecosystem. There are also the medical insurance companies, because they are also paying a lot of money for the people that need care, so it's beneficial for them if people stay healthier and more independent. And then we have the housing companies, because they want to offer their inhabitants an apartment which is barrier-free, but not just in the traditional sense. For people with dementia, for example, you need another level of “barrier-free”. And this could be the system for them. So they are really interested because they want to do something for people who no longer feel secure in their own apartments.
Then you have the concierge services, or services that complement the nursing service. You have, for example, services in the business of preparing meals, or cleaning services, or hairstylists etc. These businesses also have a strong interest in being involved in providing a holistic service.
Conclusion
The Smart Service Power project offers insight into the way in which an IoT ecosystem can be built to create the environment for growth and financial success. By bringing together an array of different service providers covering the full aged care value chain*, the project has been able to develop a lively and diverse ecosystem of businesses and authorities that can ensure the ongoing financial viability of the service.
The project undertook research into the choice of IoT platforms, the findings of which can inform other ventures. The project continues to investigate the diverse protocols for wireless communication within specific use cases. After initial market research into the acceptance of Assisted Living Systems, and positive results from live operation within its Living Lab, Smart Service Power will move into a limited number of authentic households in mid-2018 to further test acceptance levels.
To gain further tangible insights into the project, watch the following RegioStars Awards video.
Dr. Bettina Horster is Head of Business Development at VIVAI Software AG and is responsible for the area IoT (Internet of Things, Industry 4.0, M2M), and Director of IoT in eco – Association of the Internet Industry. Since 2009 she has been involved with the Internet of Things and is a pioneer in the field. She is currently also project leader for the IoT- EU project “Smart Service Power – technikgestütztes, altersgerechtes Wohnen im Quartier” (for IoT-assisted aged care in the own home), and recently won the UN NGOs Diplomatic Council “Information Society Award”, and was finalist in the UN “World Summit on the Information Society” prize.
Please note: The opinions expressed in Industry Insights published by dotmagazine are the author’s own and do not reflect the view of the publisher, eco – Association of the Internet Industry.




